button.
button.This chapter describes the procedures necessary to verify eligibility through the PROVIDER ADMINISTRATION PORTAL . Accurate eligibility verification by the provider’s office ensures the legitimacy of all encounters, avoiding lost time and effort on the part of patient, provider and CAPITATION ADJUDICATION client.
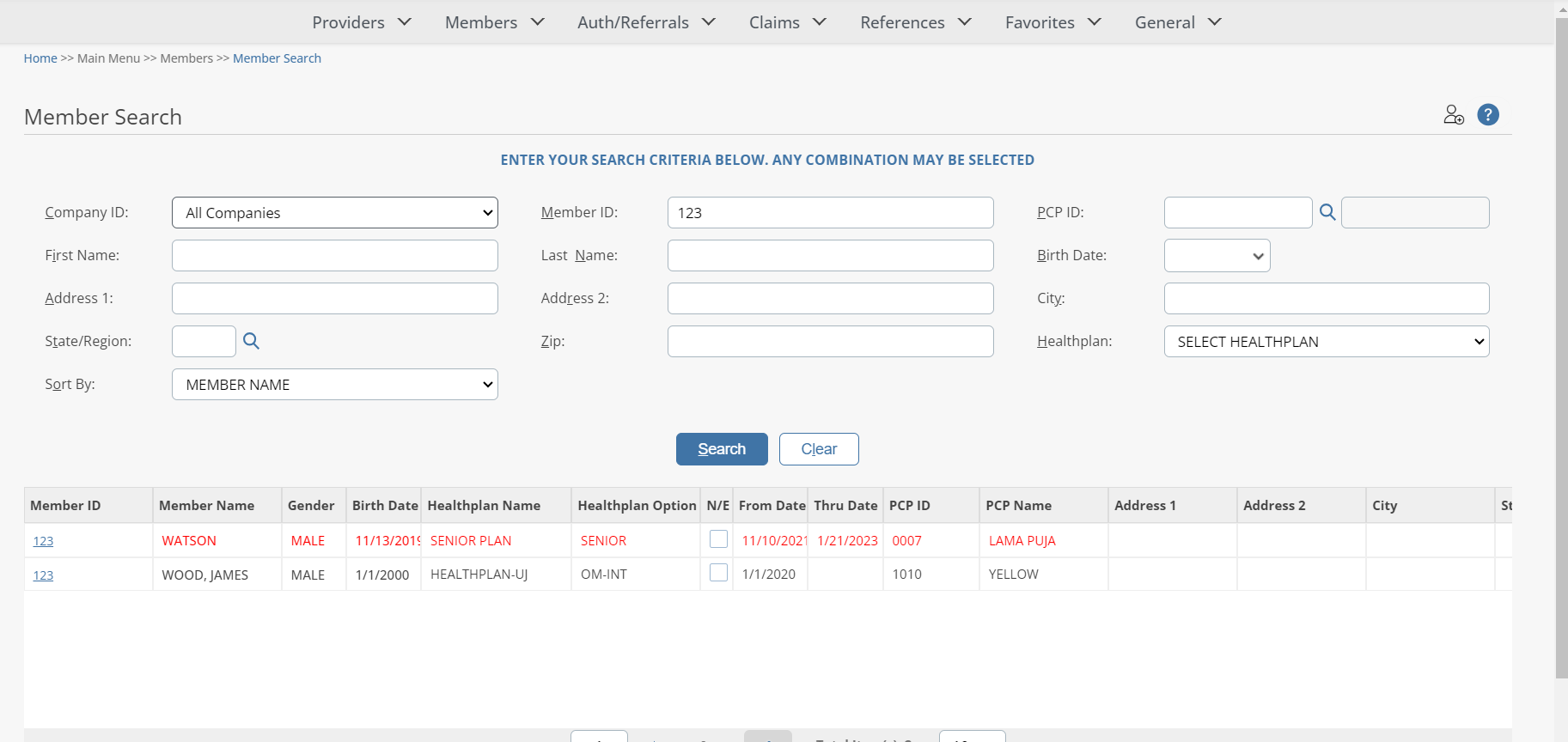
Searching For A Member
Click on Member Search in the Members section in the Main Menu to search for members.
To search for a particular member, enter any criteria you wish to narrow the results (or leave all fields empty to search ALL members) and then click on the  button.
button.
The PROVIDER ADMINISTRATION PORTAL will display the search result in the window below, sorted in your specified order (“Sort By” drop-down list). If the system does not locate any records that meet your search criteria, a message stating that “ NO RECORDS FOUND ” will display. Either replace/adjust selection criteria or click Clear and re-enter criteria.
|
Field Name |
Field Description |
|
Company ID |
Select Company ID. Click on arrow to select from drop-down list. The listing contains multiple company identifications, usually with its acronym followed by its full name. |
|
Healthplan |
To Select Healthplan. Click on arrow to select from drop-down list. The listing contains multiple Healthplan identifications, usually with its acronym followed by its full name. |
|
Member ID |
Enter the Member's unique ID number as assigned by the Healthplan or other entity. The number must be unique and can contain alpha, numeric or certain characters (* or -) values. |
|
PCP ID |
PCP (Primary Care Physician) of Member. Value defaults to ‘None Selected’, which means that the search will not be restricted to Member PCP. Searches can be limited to a specific Member PCP by using the ‘PCP ID Search’ button. |
|
Last Name |
Enter the member's last name. |
|
Birth Date |
Enter the member's date of birth by clicking on arrow to select from drop-down list. |
|
First Name |
Enter the member's first name. |
|
Address 2 |
Enter the member's address 2. |
|
Address 1 |
Enter the member's address 1. |
|
State/Region |
Enter the State/Region of the Member by clicking on Search button. |
|
City |
Enter the member's city. |
|
Sort By |
To specify the presentation order of the search results, click on the Sort By pick list and select one of the following available sort options: Member Name
Member ID
HP/Member Name |
|
Zip |
Enter the member's zip code (with or without 4-character suffix). |
Eligibility-Member Information
To display member detail, click on a member ID in the “Member ID” column (in BLUE text) within the Member Search Results window. The Notes and Memos are displayed based on the PROVIDER ADMINISTRATION PORTAL Company Configurations.
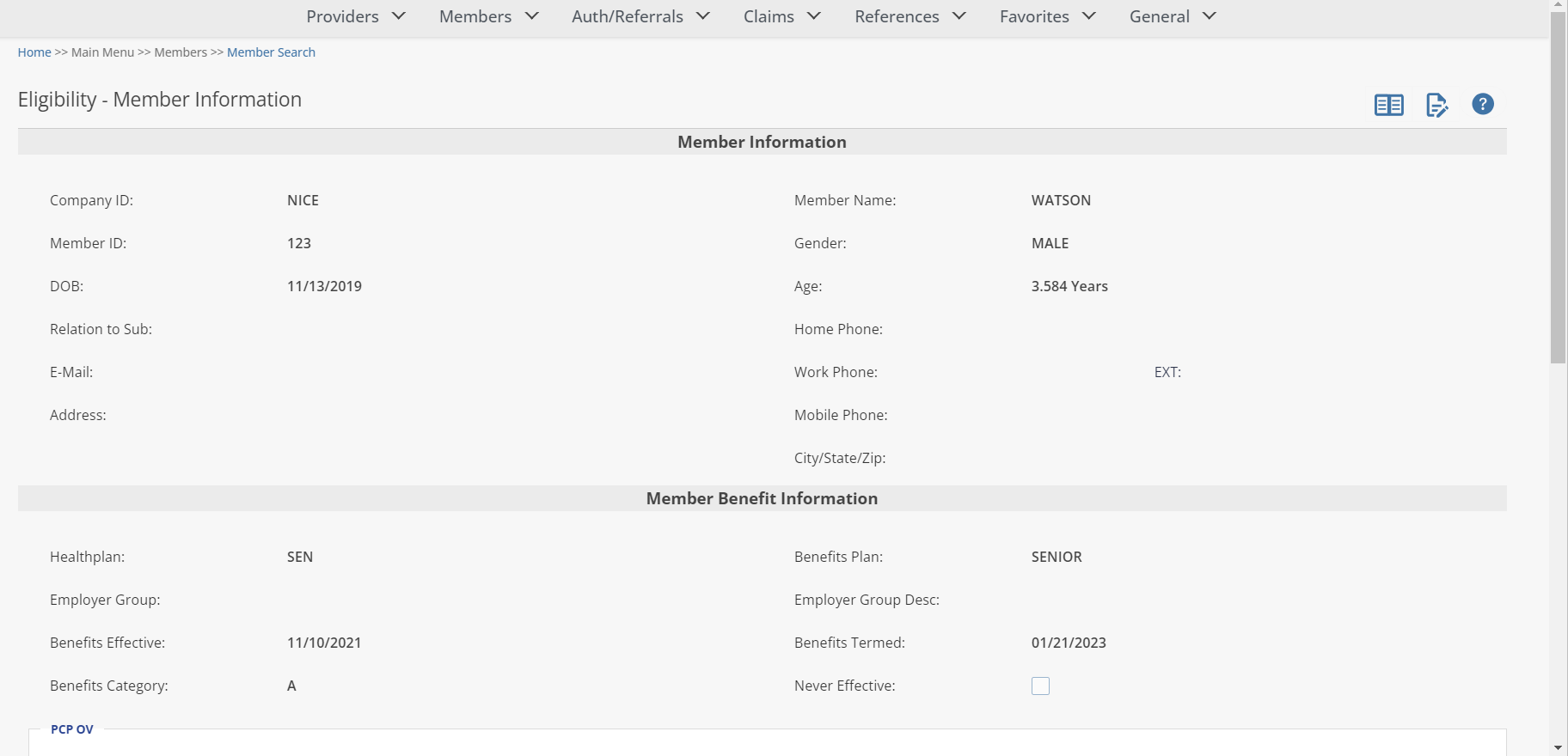
If a CAPITATION ADJUDICATION Member Alert has been defined for the member record, the sticky note icon will display to the right of the field name Member ID. Click on the sticky note to display the alert.
The Notes and Memos are displayed based on the
PROVIDER ADMINISTRATION PORTAL
Company Configuration. If a note or memo is present the icon will display red.
Member Benefits:
From the Member Information window, view the member benefits by clicking on the ![]() button.
button.
The Member Benefits window allows the user to view and track benefits and benefit limit usage. The user can view
Benefit Utilization limits, OOP and Deductible amounts,
and
Copay and Coinsurance
amounts for that member
by selecting the corresponding tab.
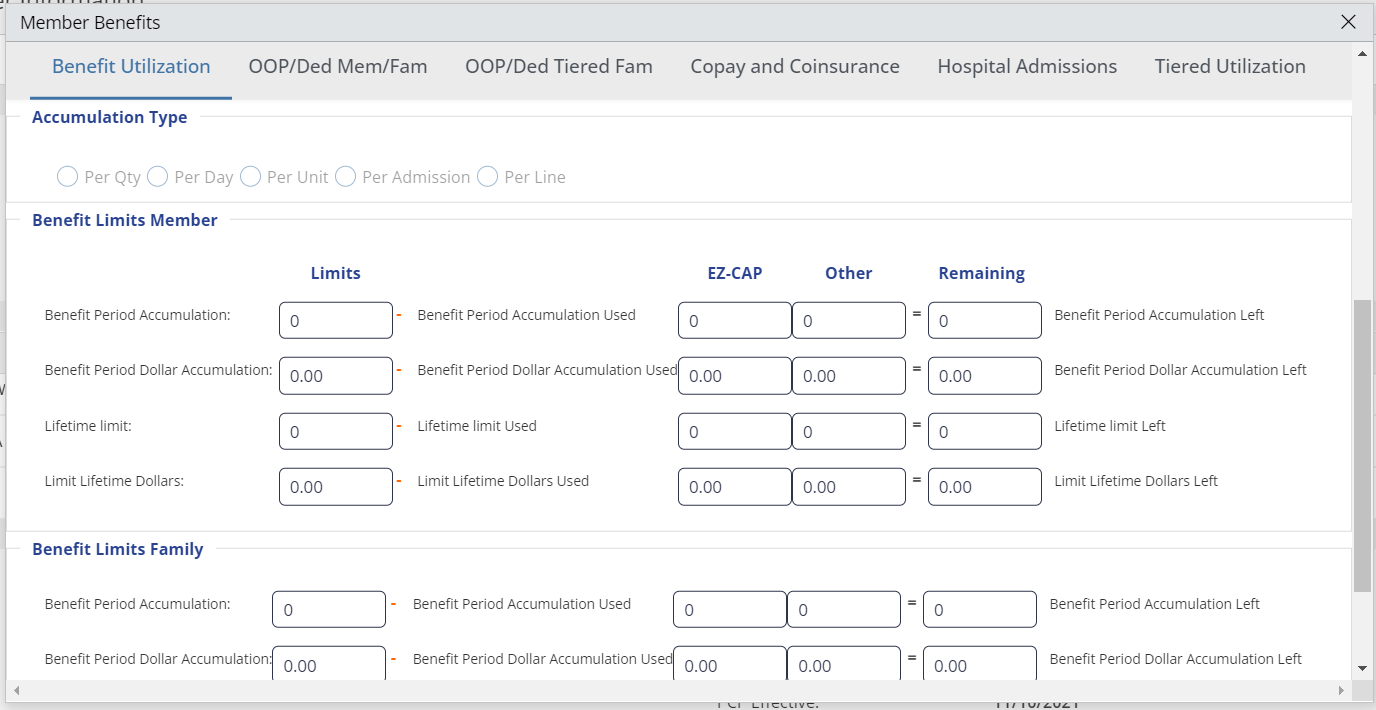
Member Benefits- 'Benefit Utilization' Tab:
The first screen is the Benefit Utilization screen. This is where the user can view the member‘s annual and lifetime unit and dollar limits and usage.
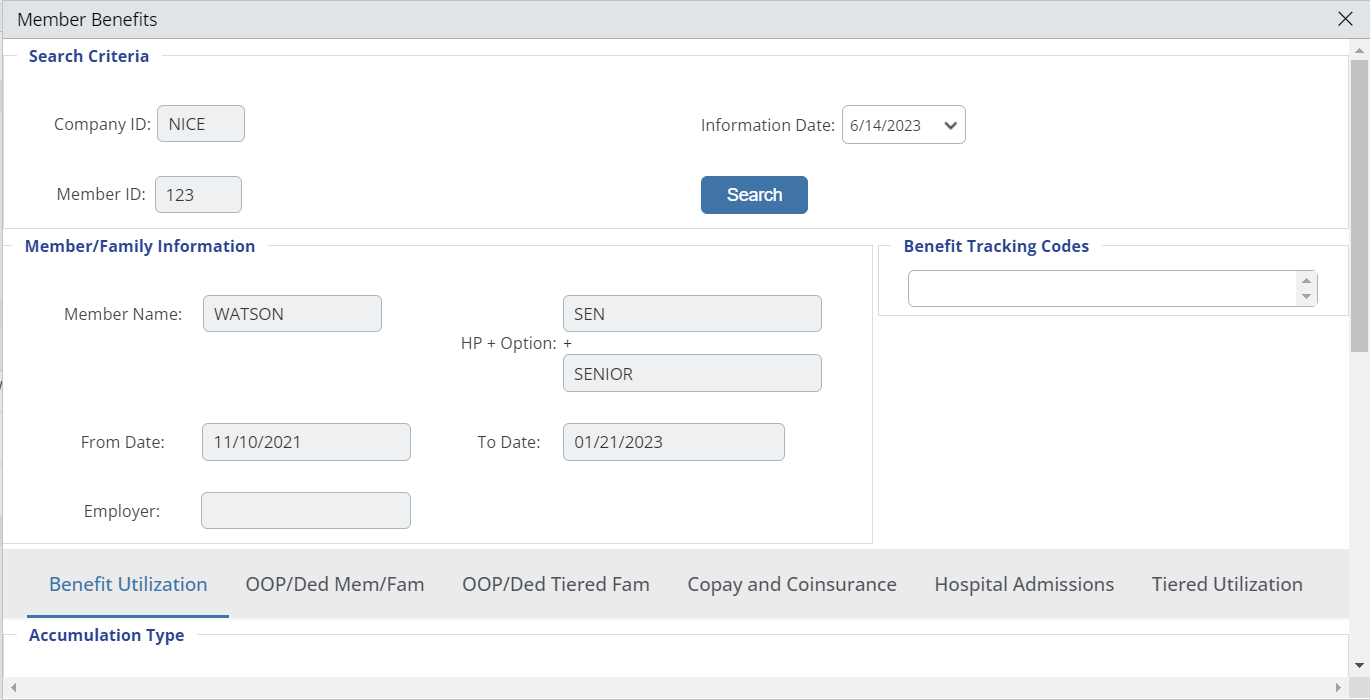
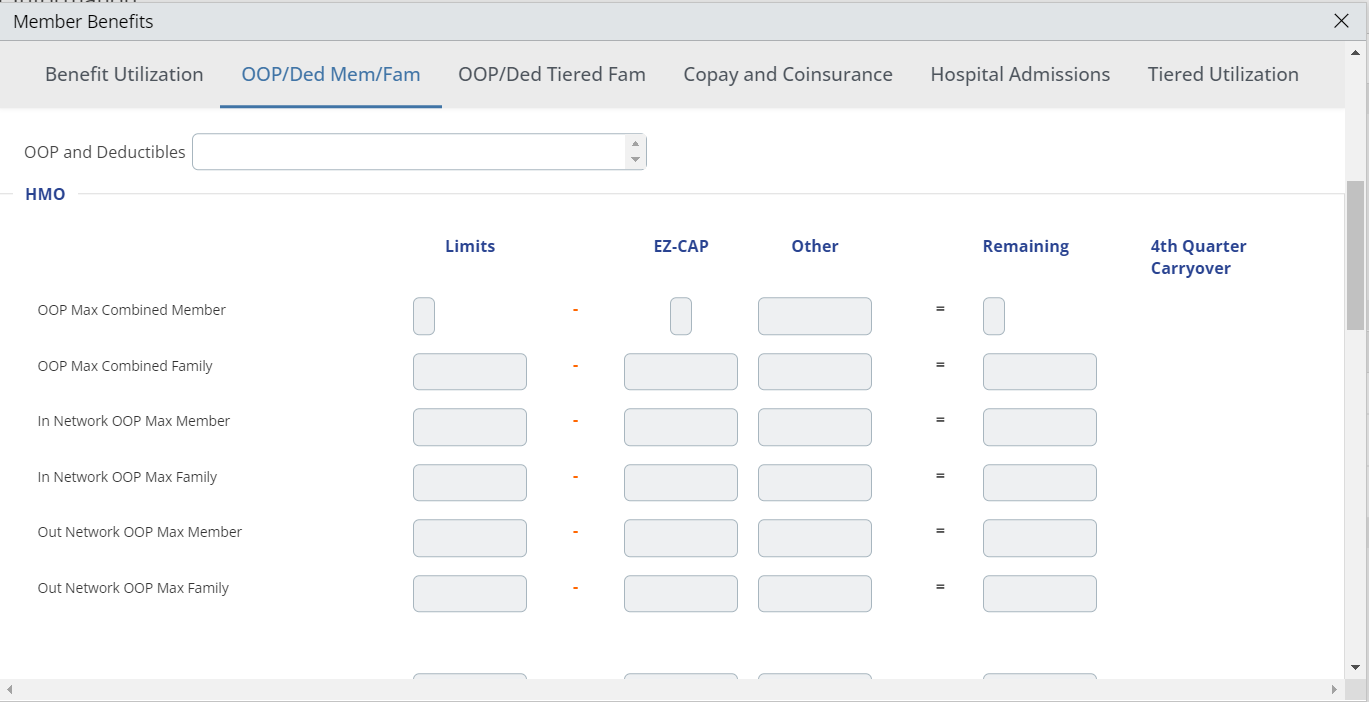
Member Benefits- 'OOP/Ded Mem/Fam' Tab
Oop
/Ded Mem/Fam
tab on the Member Benefits screen
displays OOP maximum and deductible
information for the member based on the Health plan and Option code selected.
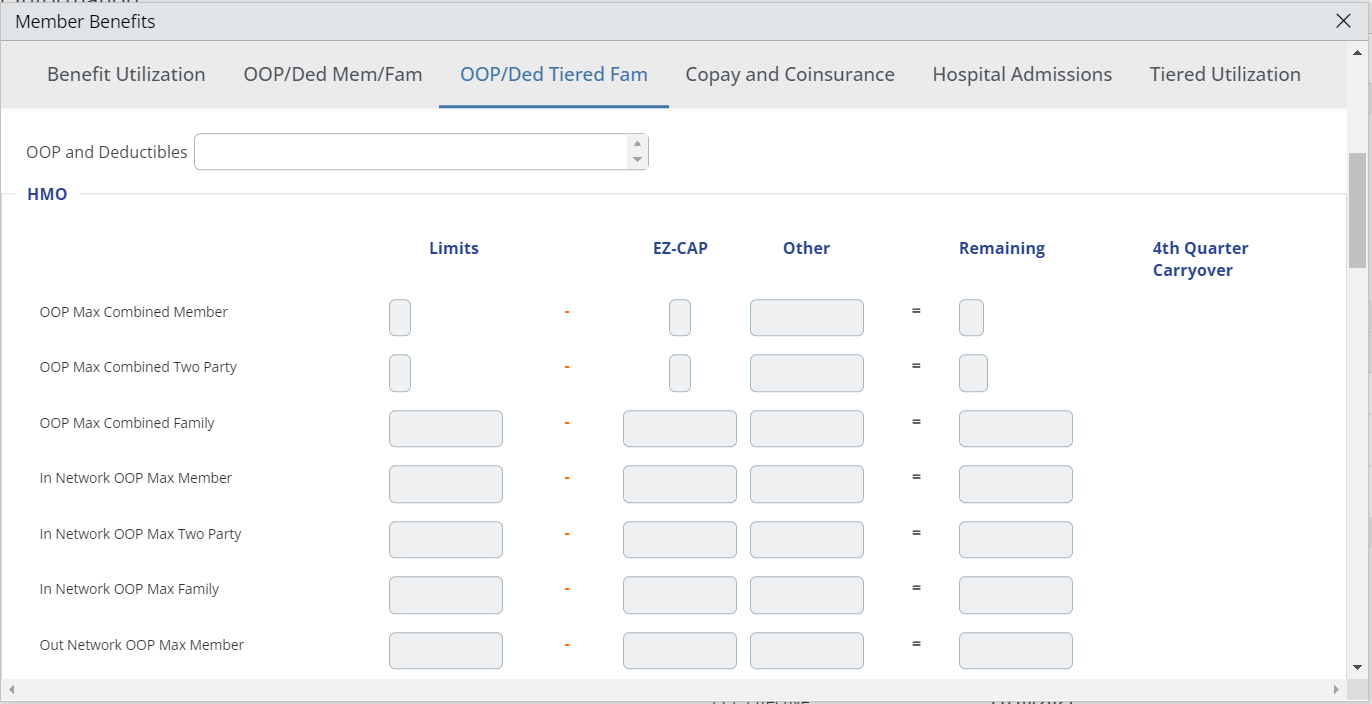
Member Benefits- 'OOP/Ded Tiered Fam' Tab
Oop
/Ded Tiered Fam
tab on the Member Benefits screen
displays OOP maximum and deductible
information for the member based on the Health plan and Option code selected.
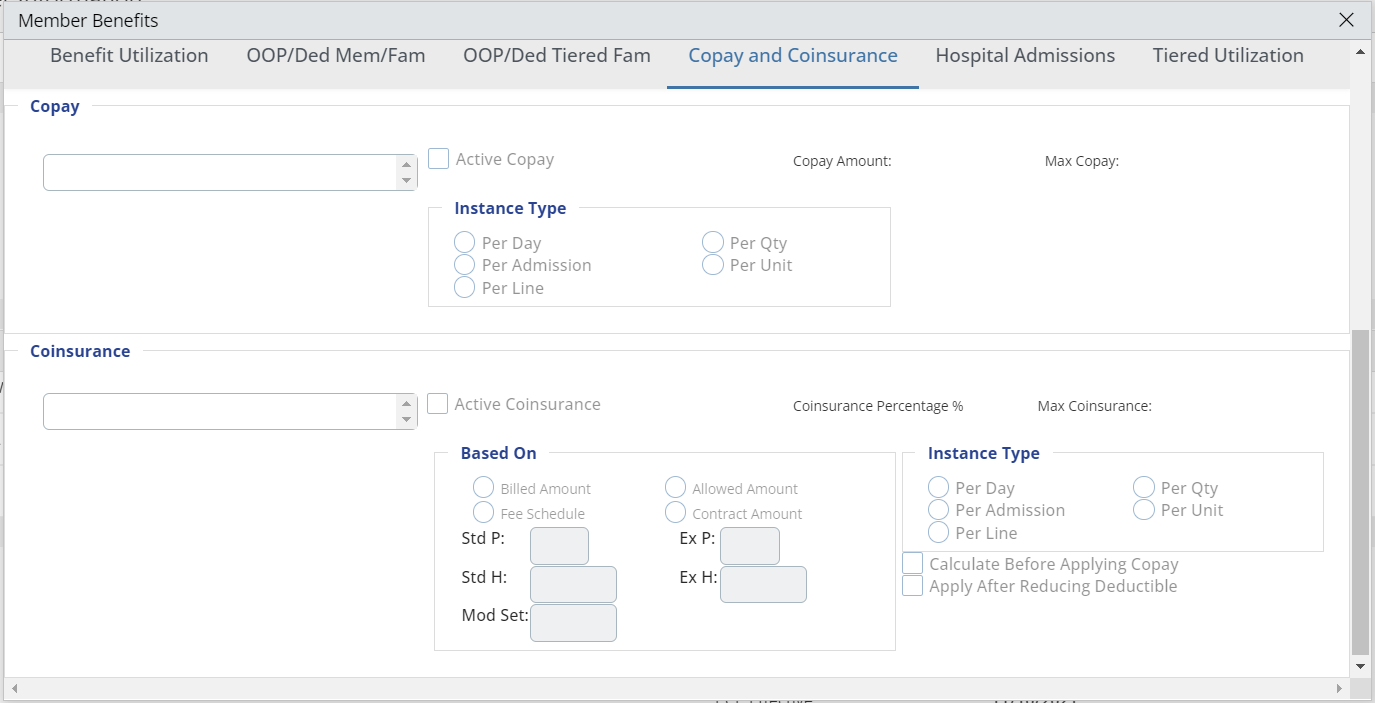
Member Benefits- 'Copay and Coinsurance' Tab
The
Copay and coinsurance tab on the Member Benefit screen displays Copay and Coinsurance information for the member based on the Health plan and Option code selected.
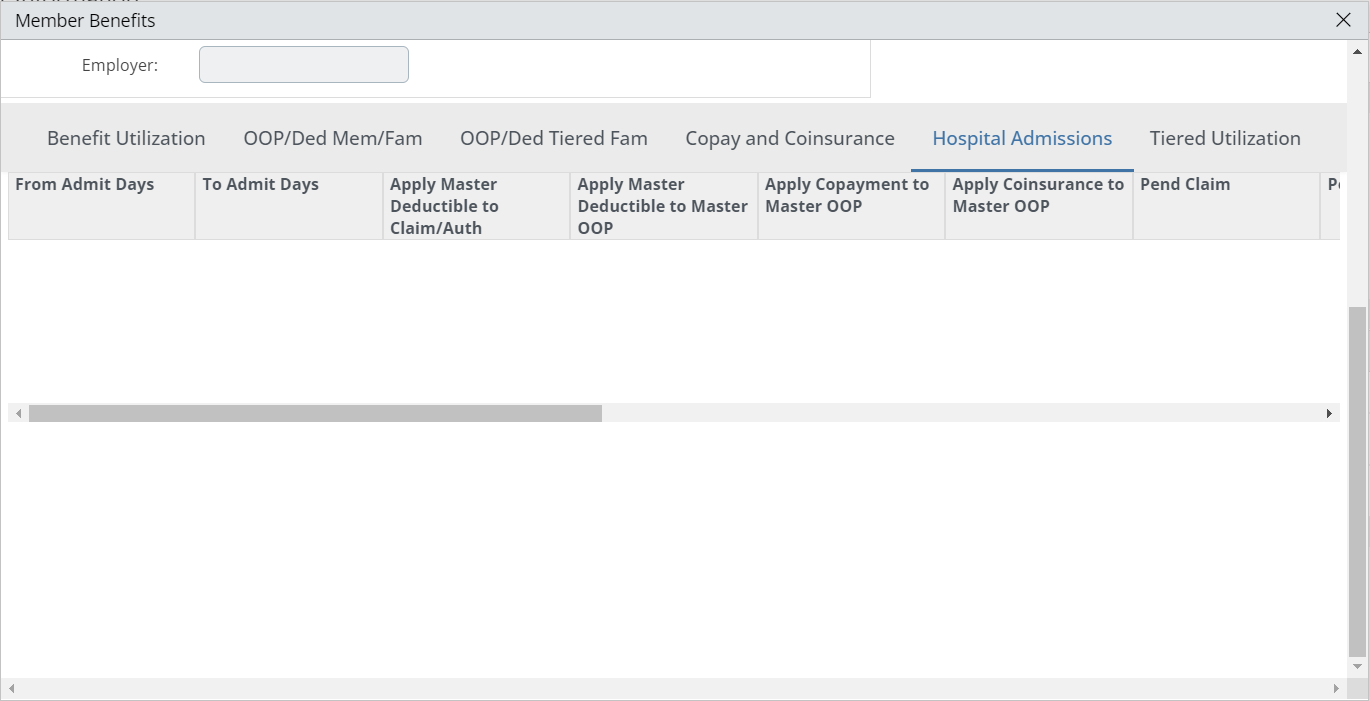
Member Benefits- 'Hospital Admissions' Tab
The
Hospital admissions tab on the Member Benefit screen
displays Hospital Admissions
information for the member if applicable.
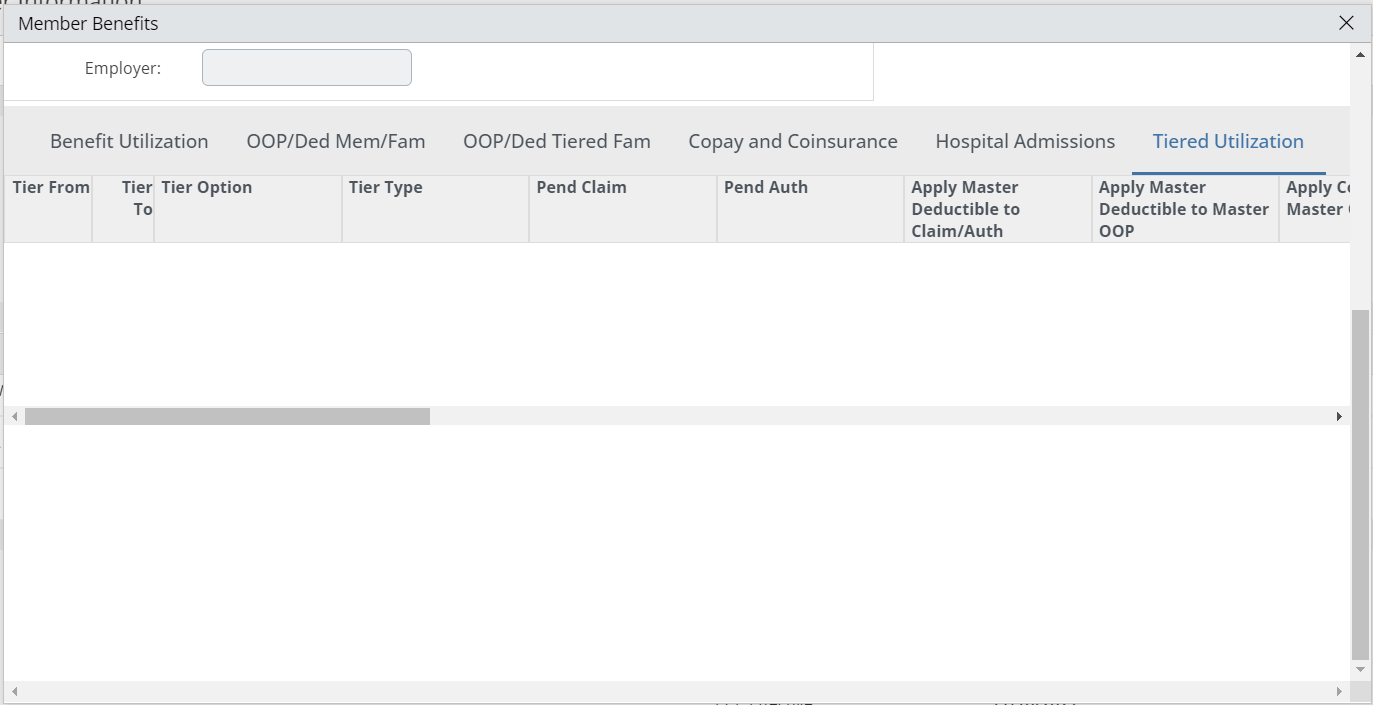
Member Benefits- 'Tiered Utilization' Tab
The
Tiered Utilization tab on the Member Benefit screen displays Tiered Utilization information for the member if applicable.
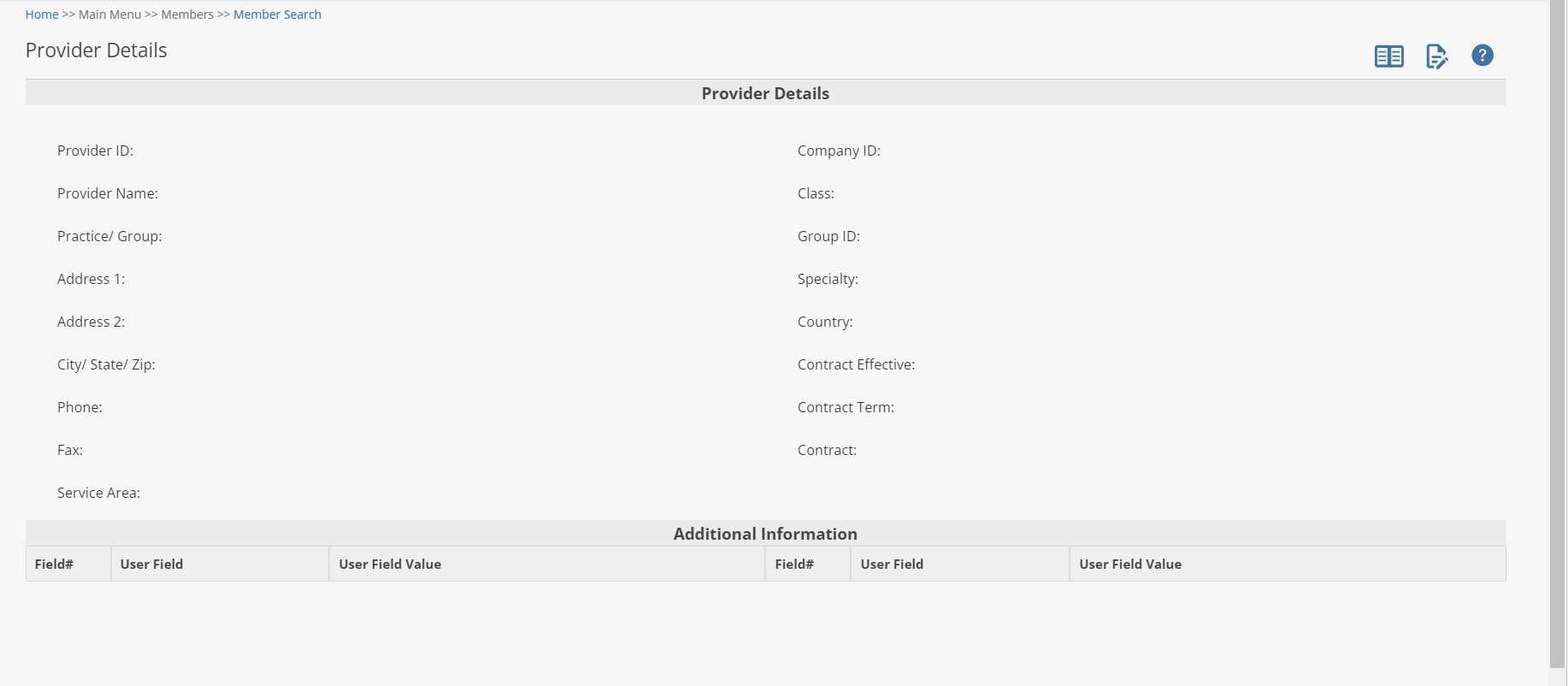
Viewing a Member's Provider Details
From the Member Information window (previous page), view detail of the member’s PCP by clicking on the PCP Name in red text in the Primary Care Provider Information section to display the Provider Detail window.
When you want to go back to the Provider Search window, use the navigation tool in the top right of the screen by clicking on the name of the screen you want.
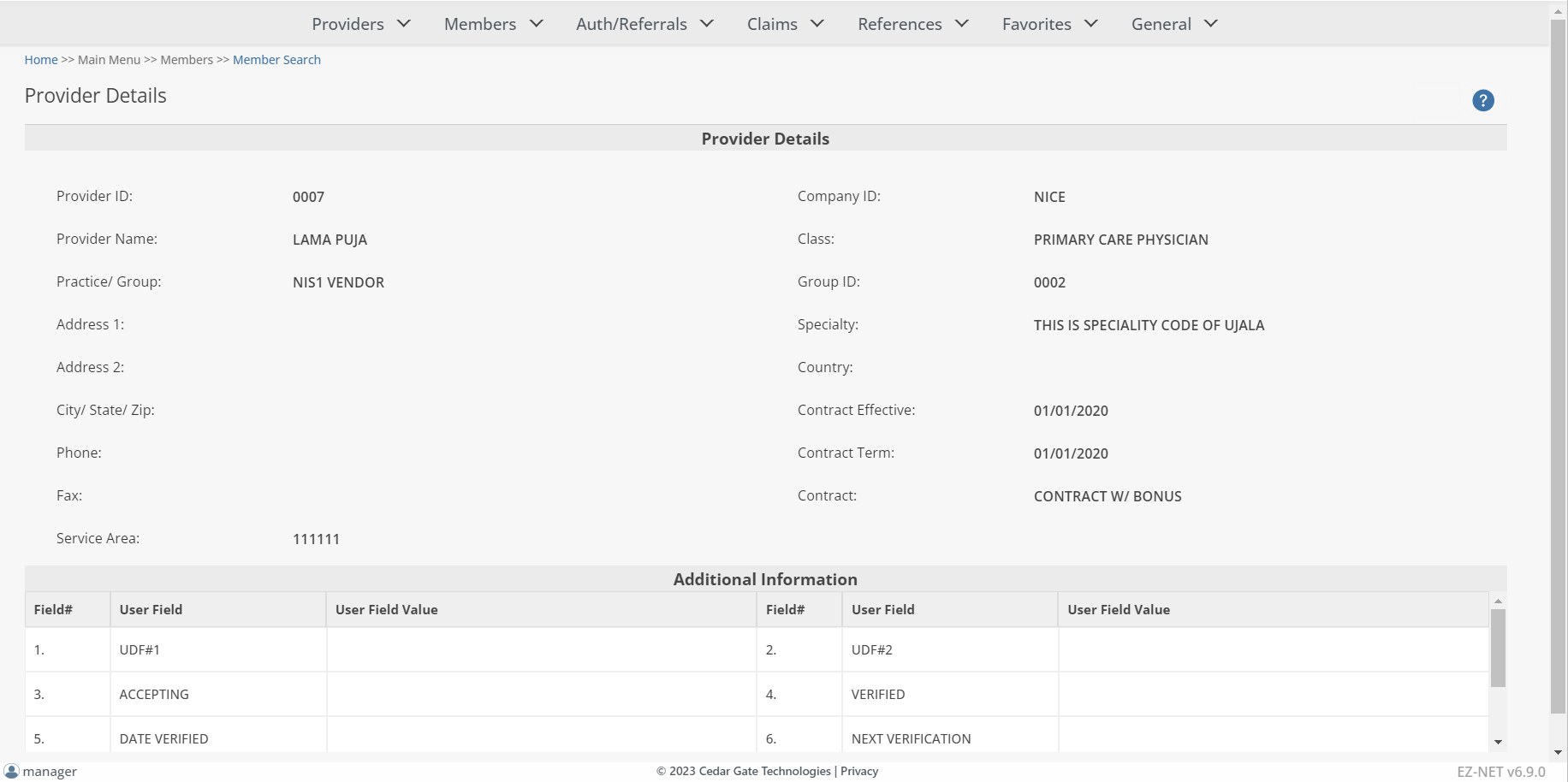
To view additional provider information, click on the Assigned Members, Health Plan Affiliations, or Office Locations buttons. (See ‘Displaying Additional Provider Information’ in the Provider Inquiry section to view these windows)
Viewing a Member's Authorization History
From the Member Information window, view the member’s auth history by clicking on the ![]() button to display the Authorization History for Member window.
button to display the Authorization History for Member window.
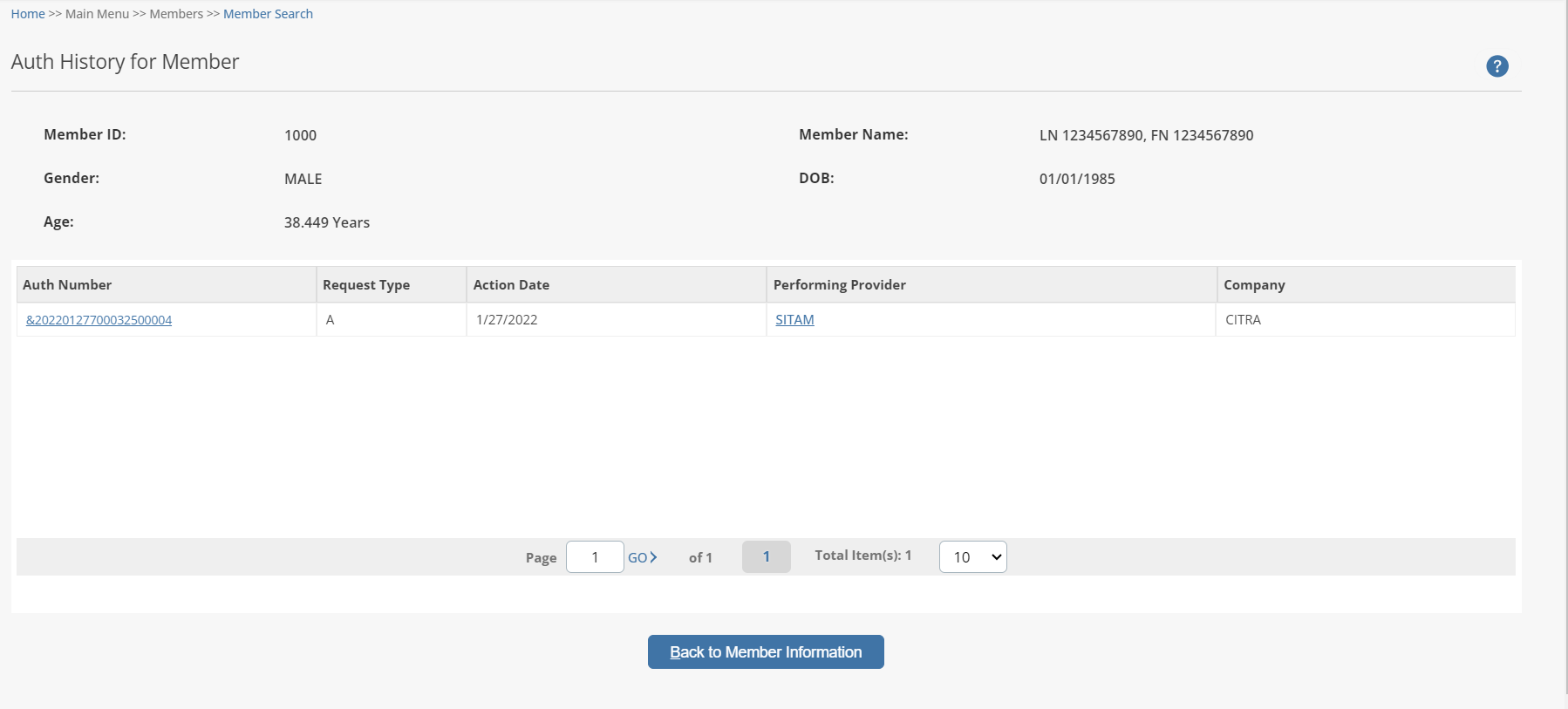
To view additional provider information, click on the Provider’s Name (under the “Ref Provider” column in BLUE text) to open the Provider Detail window.
View Additional Provider Detail from Auth History Window
To view additional provider information, click on the Provider’s Name (under the “Ref Provider” column in BLUE text) to open the Provider Detail window.